

Bart came to the University of Oxford in 2007, where he has led his independent research group since 2013. The team studies molecular imaging and therapy methods to aid cancer patients.
Tiffany is a postdoctoral researcher at the University of Oxford. She joined the Cornelissen Group as a postdoctoral researcher in January 2020, where she is working on improving 177Lu-PSMA therapy.

There are currently two main forms of radiotherapy for prostate cancer: external beam radiotherapy and brachytherapy. During external beam therapy, high-energy X-ray beams are aimed at the prostate from outside the body whereas in brachytherapy, radioactive beads are positioned inside the prostate. Radiotherapy works by damaging the DNA of the cancer cells. The cancer cells cannot repair themselves, so they are destroyed.
Unfortunately, healthy cells in the same area may also be damaged by radiotherapy, which can then lead to both short-term and long-term side-effects. Short-term side effects can include sore skin and feeling tired. Long-term side effects can include bladder and sexual changes. Also, not all cancer cells are killed, and so the cancer can grow back more aggressively.

Radiotherapy has side effects because it damages healthy cells. Targeting radiotherapy specifically to prostate cancer cells may help reduce this.
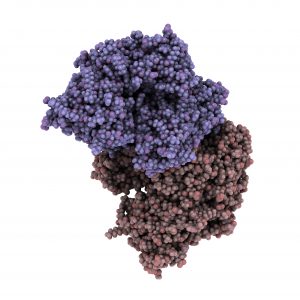
This is Prostate-specific membrane antigen (PSMA)
177Lu-PSMA is an alternative, novel form of radiotherapy to treat prostate cancer.
Prostate-specific membrane antigen (PSMA) is a protein which is found on the surface of most prostate cancer cells, but not on healthy cells. Therefore, PSMA can be used to identify which cells are cancerous and which are healthy. It can even be attached to a radioactive molecule, called lutetium- 177 (177Lu), to guide it directly to the cancer cells, without damaging healthy cells.
177Lu-PSMA is injected into the bloodstream and the radioactive molecules are taken up inside the cancer cells where they shower them with DNA-damaging radiation. 177Lu-PSMA can target multiple cancer sites at the same time so it can help those whose prostate cancer has spread to other places in the body.
177Lu-PSMA is becoming more and more available in the UK and could treat many patients with fewer side-effects than standard radiotherapy. However, it does not work for all patients at the moment.
Prostate Cancer Research funded researcher Professor Bart Cornelissen talks about his work improving radiotherapy
Bart and Tiffany are testing whether 177Lu-PSMA can increase radiotherapy effectiveness and are identifying the individuals who would benefit the most.
The researchers are exploring whether combining 177Lu-PSMA with DNA-damaging drugs could improve treatment outcomes. This type of combination therapy could lead to the treatment working more effectively and for more patients. It could also be used for patients with early stage prostate cancer. This would lead to tumour shrinkage before surgery which means patients could then undergo a less invasive surgery with fewer side effects.
The researchers will also study the biological effects of the radiotherapy. This will enable them to see how different individuals may respond to 177Lu-PSMA which could then lead to more personalised and individual treatment. This information could also be used to select which patients are suitable for treatment and which patients would not see any benefit.
The researchers will combine 177Lu-PSMA with drugs that will increase the amount of DNA damage to cancer cells. For example, they will test drugs that stop the cancer cells from being able to repair themselves. This should improve the efficacy of 177Lu-PSMA so that it will work better and for more prostate cancer patients leading to higher survival rates. They will be testing 177Lu-PSMA with approximately 1,000 different drugs in the hope of finding a successful combination.

This project is still in the early stages but the researchers have begun to test different drug combinations with 177Lu-PSMA. In the next stage of their research, the researchers will use SPECT imaging to measure the DNA damage following treatment with 177Lu-PSMA. This will enable them to see how effective this type of radiotherapy is at treating prostate cancer. They hope to find successful combinations that could lead to clinical trials and eventually improved and personalised radiotherapy treatment for prostate cancer patients.
This project is a collaboration between researchers and clinicians from the University of Oxford and the Oxford University Hospitals Trust. They will also be collaborating with a researcher from the Erasmus University Medical Centre in the Netherlands.
“Late-stage prostate cancer remains challenging to treat, especially cancer that has spread to other organs, and is resistant to testosterone removal therapy. Using this PCR award, we will investigate novel therapy combinations for prostate cancer, to increase tumor kill, while reducing unwanted side-effects. This award will allow us to perform these studies on an unprecedented scale, an exciting prospect. It increases the likelihood we will find a potent combination of therapies, improving the prospects for long-term cures in this group of cancer patients.
Professor Bart Cornelissen
University of Oxford